In mid-November, CMS published the CY 2019 Quality Payment Program (QPP) Final Rule which included numerous updates to the Merit-based Incentive Payment System (MIPS) for Year 3 of the QPP (2019 Reporting).
MIPS Eligibility
CMS added new eligible clinician types for 2019 reporting: physical therapist, occupational therapist, qualified speech-language pathologist, qualified audiologist, clinical psychologist, and registered dietitian or nutritional professional. MIPS eligible clinicians continue to also include physicians, physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists.
There was a change made to the low-volume threshold (LVT) for 2019 reporting as it now includes a third criterion. A clinician or group will be excluded from 2019 MIPS reporting if the clinician or group (1) bills $90,000 a year or less in Medicare Part B allowed charges for covered professional services, (2) provides care to 200 or fewer Medicare Part B-enrolled beneficiaries a year OR (3) provides 200 or fewer covered professional services under the Physician Fee Schedule (PFS). This change to the low volume threshold will exempt additional providers/groups from being eligible for MIPS reporting. However, these providers/groups have the option to opt-in to MIPS if they meet or exceed at least one, but not all three, of the LVT criteria and qualify for the MIPS payment adjustment or these providers/groups can voluntarily report and not qualify for the MIPS payment adjustment.
Reporting Options
In Year 3 of MIPS, providers continue to have the option to report as an individual defined by TIN/NPI, as a group defined by TIN or as a virtual group, consisting of solo practitioners and groups of 10 or fewer eligible clinicians who aggregate their reporting data virtually to report to MIPS. The virtual group election period for 2019 reporting runs from October 1 through December 31, 2018.
Submission Terminology
CMS finalized 3 new terms related to submissions: Collection Type, Submitter Type, and Submission Type. Collection type refers to a set of quality measures with comparable specifications and data completeness criteria including, eCQMs, MIPS CQMs (formerly Registry Measures), QCDR measures, Medicare Part B claims measures, CMS Web Interface measures, the CAHPS for MIPS survey measure, and administrative claims measures. Submitter type is the MIPS eligible clinician, group, or third-party intermediary acting on behalf of a MIPS eligible clinician or group that submits data on measures and activities. Lastly, submission type is the way in which the submitter type submits data to CMS such as direct, log in and upload, log in and attest, Medicare Part B claims, and the CMS Web Interface.
Facility-Based Reporting
CMS finalized Facility-Based Reporting for 2019 MIPS Reporting. For facility-based scoring, the measure set for the FY2020 Hospital Value-Based Purchasing (VBP) Program will be used for the 2019 MIPS performance period. A MIPS eligible clinician qualifies for facility-based reporting if he/she furnishes 75% or more of their covered professional services in an inpatient hospital, on-campus outpatient hospital, or an emergency room, with at least a single claim billed for the inpatient hospital or emergency room. A facility-based clinician will be attributed to the hospital at which they provide services to the most Medicare patients. A group qualifies for facility-based reporting if 75% or more of the MIPS eligible clinicians’ NPIs billing under the TIN are eligible for facility-based measurement as individuals. A facility-based group will be attributed to the hospital at which a plurality of its facility-based clinicians is attributed.
Facility-based measurement is automatically applied to MIPS eligible clinicians and groups who are eligible and have a higher combined quality and cost score, when compared to their regular MIPS quality and cost submission, should they submit. While there are no submission requirements for individual clinicians, a group must submit data in IA and PI to be measured as a group under facility-based measurement. Quality and Cost performance category scores are determined by using the percentile performance of the facility in the Hospital VBP program for the specified year and awarding a score associated with that same percentile performance in the MIPS Quality and Cost performance category scores for those clinicians who are not scored using facility-based measurement. If a hospital did not receive a VBP score for any reason, then facility-based reporting would not be a reporting option.
MIPS Performance Categories
Cost
In Year 3 of QPP, CMS has finalized that Cost will be weighted at 15% of the Total MIPS Score, an increase from 10% in Year 2. In addition to the two administrative claims-based measures included in the 2018 cost score, Medicare Spending per Beneficiary (MSPB) and total per capita cost, CMS finalized the addition of 8 episode-based measures. An individual MIPS eligible clinician or group will be scored on these measures if they meet the case minimums. Since these measures are scored using administrative claims, individuals and groups are not required to submit any information for the Cost performance category. The performance period is the full calendar year.
Quality
In Year 3 of the QPP, the Quality performance category will be weighted at 45% instead of 50% to account for the increased weighting of the Cost category. An eligible clinician or group must still report on 6 measures, including 1 outcome measure or high priority measure for the full calendar year. The data completeness requirement remains at 60% and measures that do not meet data completeness will only receive 1 point; small practices will continue to receive 3 points. Improvement for the Quality measures will continue to be measured at the performance category level. New in Year 3, any MIPS eligible clinician or group in a small practice will receive 6 bonus points in the Quality performance category numerator so long as the individual or group reports on at least 1 quality measure. Lastly, beginning with 2019 MIPS reporting, CMS is allowing the use of a combination of collection types for the Quality performance category.
Topped Out Measures
Measures are considered topped out when meaningful distinctions and improvement in performance can no longer be made. Topped out measures will be removed and scored on a four-year phasing out timeline. Measures that are deemed topped out for at least 2 consecutive years and have benchmarks will receive up to 7 points, as opposed to 10. CMS finalized an additional factor beginning with Year 3 for extremely topped out measures, in which measures with an average mean performance within the 98th and 100th percentile range can be proposed for removal in the next rule-making cycle without following the 4-year lifecycle process.
Promoting Interoperability
CMS had previously renamed the MIPS Advancing Care Information Category (ACI) to MIPS Promoting Interoperability (PI). Beginning with 2019 MIPS reporting, CMS has finalized a new performance-based scoring methodology, replacing the current PI structure of base and performance measures. Beginning with CY 2019 reporting period, CMS requires that all hospitals attesting to these programs use EHR technology certified to the 2015 Edition.
Under this new PI Program methodology, MIPS clinicians and groups will be required to report certain measures from each of the four objectives, with performance-based scoring happening at the individual measure-level. Each measure will be scored based on the hospital’s performance for that measure, except for the Public Health and Clinical Data Exchange objective which requires a yes/no attestation. Each measure score would be added together to calculate the total PI score of up to 100 possible points.
To earn any score in the PI Program, CMS finalized that clinicians and groups would have to attest that they completed the actions included in the Security Risk Analysis measure at some point during the calendar year and must submit a numerator and denominator or yes/no for all required measures. For measures that include a numerator and denominator, the hospital must submit a numerator of at least one. The numerator and denominator for each measure will translate to a performance rate for that measure contributing to the total PI score.
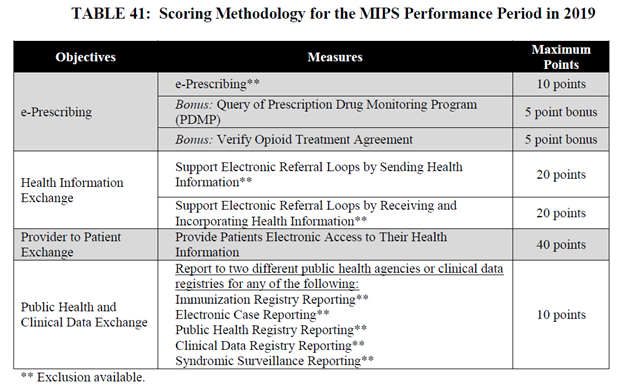
CMS finalized four objectives for the 2019 MIPS PI Category: e-Prescribing, Health Information Exchange, Provider to Patient Exchange, Public Health and Clinical Data Exchange with 6 required measures and 2 bonus measures. CMS has removed several measures from the 2018 PI program for hospitals but has retained e-Prescribing and the Public Health and Clinical Data Exchange measures. CMS renamed ‘Send a Summary of Care’ to ‘Supporting Electronic Referral Loops by Sending Health Information’ and ‘Provide Patient Access’ to ‘Provide Patients Electronic Access to their Health Information’. CMS finalized a new measure, ‘Support Electronic Referral Loops by Receiving and Incorporating Health Information’, which combines ‘Request/Accept Summary of Care’ and ‘Clinical Information Reconciliation’. CMS also finalized two new measures as bonus measures: ‘Query of Prescription Monitoring Program (PDMP)’ and ‘Verify Opioid Treatment Agreement’. The measures and corresponding available points for scoring are outlined in the following table.
Improvement Activities
For Year 3 of the QPP, CMS did not make any changes to the number of activities MIPS eligible clinicians must report to achieve a total of 40 points. CMS did, however, add 6 new activities, modified 5 existing activities, and removed 1 existing activity. CMS also removed the PI Bonus that was available for Certified EHR Technology (CEHRT) eligible Improvement Activities.
Additional Bonus Points
For 2019 MIPS reporting, clinicians can continue to earn up to 5 bonus points for the treatment of complex patients based on a combination of the Hierarchical Condition Categories (HCCs) and the number of dually eligible patients treated.
MIPS Scoring, Performance Threshold, and Payment Adjustment
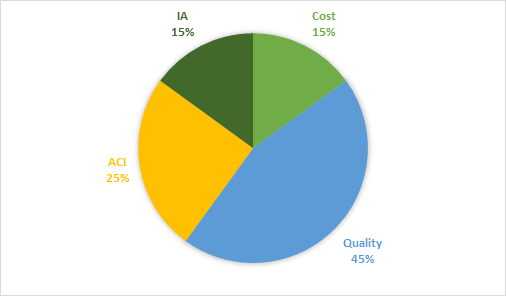
For 2019 MIPS reporting, the final MIPS score will be based on the four performance categories and their corresponding weights.
- Cost: 15%
- Quality: 45%
- Advancing Care Information: 25%
- Improvement Activities: 15%
For 2019, the performance threshold has been set at 30 points, an increase from the 2018 performance threshold that was set at 15 points. The exceptional performance threshold increases to 75 points, an increase from 70 points. MIPS eligible clinicians and groups with a MIPS score of less than 30 points will receive a negative 7 percent payment adjustment in 2021. Positive payment adjustments will be made while ensuring budget neutrality.
Should you have questions about MIPS or need help with your MIPS reporting, please contact us.

